The Current Canadian Health Care System
Ever since I was a medical student about 20 years ago, I remember “people” talking about how our Canadian health care system was faltering, how the waiting times for access to medical care were way too long, and how we needed a major transformation in our health care system to make it sustainable.
Well, guess what? Twenty years later and “people” are still saying the same things.
And it’s not just the “people.” The stats are saying the same things as well. In a recent report from the Canadian Institute for Health Information (CIHI), the experiences and perceptions among a random sample of Canadians ages 18 and older were compared with that of 10 other countries: Australia, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom and the United States. And here’s the bottom line:
Canadians reported the longest wait times of all 11 countries to see a family doctor, to see a specialist, and at the emergency department.
In fact, 1 out of every 5 Canadians reported waiting 7 or more days to see a family doctor the last time they needed medical attention; 1 out of 3 Canadians reported waiting 4 or more hours the last time they went to the emergency department; and 1 of out 2 Canadians reported waiting 4 or more weeks to see a specialist.
This is pathetic.
Interestingly, here is the good news: once a person finally does access the Canadian health care system, they are generally happy with the quality of their care. 74% of Canadians say they received excellent or very good care from their regular doctor, which is above the 11-country average of 65%. The problem in Canada is not the quality of care, but rather access to care.
As the Globe in Mail reported, “Canada’s health-care system suffers from what experts call ‘code gridlock’ – provision of care moves at a glacial rhythm because of clogs in the system.” Nursing home beds are full and home care hours are limited so thousands of patients who no longer need hospital care can’t actually leave the hospital because they have no place to go. Consequently, hospital beds are not available for patients who might need them acutely or for elective surgeries, so these patients languish on gurneys in the halls of the ER or at home hoping that their elective surgery will not be cancelled for the second or third (or fourth!) time.
In the past the solution to the access dilemma was to throw more money and health care practitioners at the problem. The result? “Canada has more physicians, in absolute numbers and per capita, than ever before, with seemingly little impact on access.” This approach is not working. So what does work?
What is Voice-First Technology?
Amazon Alexa. Google Assistant. Microsoft Cortana. Samsung Bixby. Apple Siri. IBM Watson. The list goes on and on. All of the major technology companies are investing billions of dollars into developing artificial-intelligent voice-first personal assistants that we simply talk to.
The adoption rate of these voice-first assistants is faster than that of the mobile phone a decade ago.
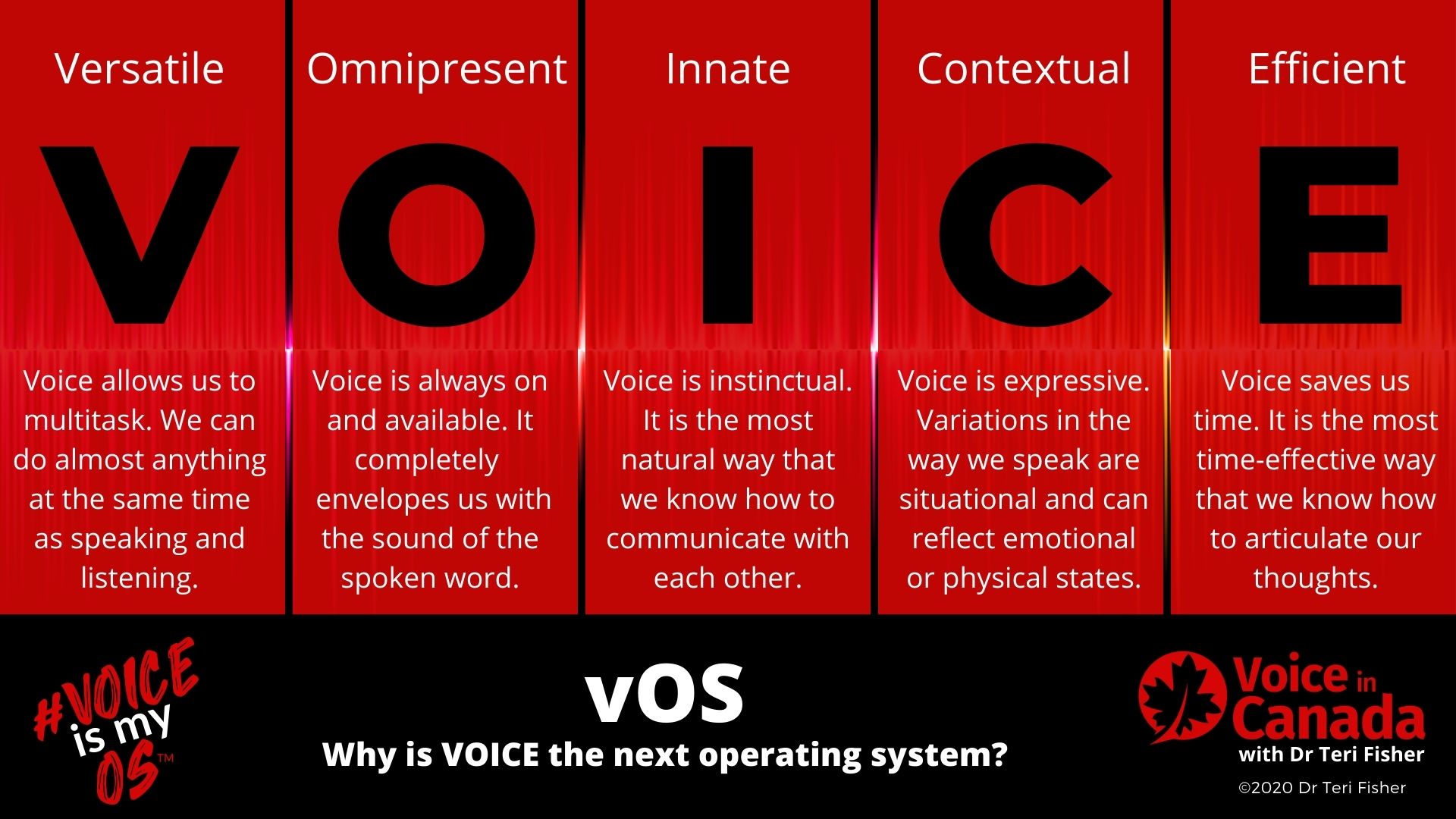
The reason for this is that in the past humans had to adapt to technology to be able to communicate with their computers and devices – just recall the original typewriter, and then computer keyboard and mouse for examples of this. Then we were able to remove the physical keyboard and “communicate” with our devices through a touchscreen. And now, we have finally arrived at a time when the technology is adapting to us, to our most natural method of communication – our voices.
This is not a fad. Voice-first technology is becoming the operating system of the present and future.
It is here now and this will disrupt the way we do everything in every sector to one degree or another. Witness the radical transformations in everything from voice-assisted home automation to industry customer service chat-bots; from ordering your pizza by voice to ordering your next car ride, to name just a few.
So, how does this pivotal time in our history relate to our Canadian health care system? Well, there are many more questions than answers at this point, but these answers are starting to become apparent in other countries already.
Currently, in Canada (and elsewhere), there is a lot of discussion about the concept of “the right health care at the right time at the right place” to try to ease the pressure on the health care system. And this is precisely where voice-first technology has the ability to completely disrupt and transform the Canadian health care system.
Let’s tackle each of these elements one by one.
“The Right Health Care”
As I have already stated, most Canadians believe they are getting quality care when they eventually do get access the health care system. However, could this be improved?
To answer that, we have to first define “the right health care.” As far as I am concerned, the right health care is defined as the most cost-effective medical advice or intervention that can be obtained under the particular circumstances that results in improved health outcomes. That may mean seeing a doctor, but that might also might mean being prompted to take one’s medication. Maybe it means getting 30 minutes of exercise or maybe it means seeing a therapist. Herein lies a problem with the system – how does a patient know definitively how to obtain “the right care” without asking a knowledgeable person?
The British Columbia Ministry of Health has tried to tackle this problem by providing an 8-1-1 phone line, operated by HealthLink BC. 8-1-1 is a free-of-charge (to the patient) provincial health information and advice phone line available in British Columbia. By calling 8-1-1, individuals can speak to a health service navigator, who can help find relevant health information and services or connect the patient to certain allied health care professionals. One of the main problems with this is that there is some inherent friction to calling a person, and in some cases, the patient may feel that the call is not important and may feel that he/she is a burden on the system.
Now what if there was an artificial-intelligent (AI), voice-first personal assistant in your home, a health navigator so to speak, that you could access anytime you wanted? What if you could simply speak to your personal health navigator, one that knows who you are, what your medications and allergies are, what your chronic health conditions are, and who your personal health care providers are? What if your navigator could ask you a few questions about your current condition and then tell you how or where to obtain the right health care for your situation?
Maybe it could even provide the “right health care.”
Perhaps the navigator could ask you questions about your current flu-like symptoms, help you determine that you probably have a common cold and tell you that the “right care” is to get into bed with some soup, and get some rest (and not clog-up the emergency department).
This would save the system financially, not just by replacing the 8-1-1 operators, but also by potentially eliminating the need for unnecessary visits to the doctor or emergency room.
Sure, some safeguards would have to be in place to deal with emergencies – that goes without saying – and perhaps getting the right care is actually having the navigator automatically call 9-1-1. But just imagine if every household had a health navigator that truly helped individuals get the “right care” for their particular situation?
“The Right Time”
Now, here is the BIG problem with the Canadian health care system. Again, it has been well documented that Canada is scoring well below par when it comes to timely access to health care. So how could a digital AI voice assistant help with this?
Well, starting in the home again, a health navigator, based on your personal history and your particular situation, could advise you to stay at home, make an appointment with your family doctor in the next week, on the same day, go to the emergency department, or even directly connect you with 9-1-1.
Right off the bat we would effectively have a triage “nurse” in every home that could determine the urgency of the situation, helping to direct the Canadian health care resources of the population, but on an individual basis.
We haven’t even touched on the fact that the incredible data that could be collected through this system (yes, there are privacy issues that must be worked out here) could then be used to further optimize our medical system.
What about access to specialists? How could this be improved? Imagine if an AI voice-first medical office assistant was present in each doctor’s office. A human medical office assistant could have a dialogue with the AI office assistant to determine which orthopedic surgeon, for example, currently had the shortest wait time. Perhaps the AI could then schedule the appointment, triage the appointment based on the particular diagnosis (see above) and then communicate with the patient’s personal health navigator at home to make the process seamless, efficient, and save costs to the system. Perhaps the referring physician could even talk to the AI assistant in the exam room during an appointment with the patient to generate the referral in real time. The physician and the patient could be immediately informed of the wait-time and everyone would be on the same page.
“The Right Place”
It is not unusual in Canada (in fact it is commonplace) for a patient to attempt to make an appointment with his/her family doc and then encounter a long wait time. Because of the wait time, the patient might even end up in an emergency room, not because the situation is an emergency, but because the person did not know where else to get timely care. Clearly, the emergency department is not “the right place.”
How could a voice-first assistant help in this case? First, as we’ve discussed, a personal assistant could help to triage and direct patients to the right place. If this practise became the standard of care, one would expect that the appropriate medical problem would be directed towards the right place for the required intervention.
Consider the elderly aging parent that wants to remain in her own home instead of moving to a care home. What is the right place for this person? Maybe if this Canadian citizen had the support of a personal AI health navigator who could provide guidance about when to take her medications and to make sure that she was eating a healthy diet, this senior could remain in her home that much longer.
In the eyes of the senior, home is certainly the “right place.”
As another example, consider the patient who is unsure if he/she requires vaccinations prior to going on a vacation. Where is the right place to obtain this advice and the vaccines – a doctor’s office, a community health clinic, a travel clinic, or somewhere else? The patient could discuss this with their health navigator, who could confirm what vaccines are due and then suggest the “right place” and book an appointment to obtain the vaccines in a timely manner.
Voice-First Technology is the Future of Canadian Health Care
These examples are just the tiny tip of the iceberg. Imagine how voice-first technology could transform medical record keeping and EMRs within the Canadian health care system. What about those living with disabilities or in group homes? What about preventative health programs administered through voice-first assistants in each home? Health care professionals could use AI assistants in pre-op and post-op care to check-in with patients or to answer frequently asked questions. AI health assistants could be used in chronic disease management (e.g. “what is your blood sugar today?”). What about the nurse that needs to record every single pill that he administers during a shift in a hospital? What if he could just talk to his AI assistant? How about the physiotherapist that wants her patient to do a set of exercises – could the assistant talk the patient through the activity, emphasizing certain key aspects of the rehab? Or what about the use of voice assistants in teaching medical students and residents in simulated situations? The possibilities for applications of this technology are limited only by our imaginations.
And here’s the kicker: this technology already exists… just not in Canada.
Canada is already falling behind when it comes to voice-first technology. It’s time to get moving, Canada. It’s time that we transformed our health care system.
Twenty years ago, as a medical student, I remember “people” saying that the Canadian health care system was faltering. Could voice-first assistants finally provide the “right care” at the “right time” in the “right place” that we have been waiting for? I think so. As with everything else, time will tell. I sure hope today’s medical students aren’t having a similar discussion 20 years from now about what could have been.